

The history of closed sucking
In the treatment of critically ill patients, intratracheal suction is an important measure, the purpose of which is to timely absorb the secretions of the respiratory tract to maintain artificial airway patency, ensure adequate ventilation and adequate gas exchange, maintain ventilation function, prevent And the treatment of lung infections and other important. The earlier intratracheal suction was performed by OPEN ENDOTRACHEAL SUCTION (OES). The artificial airway was separated from the ventilator during each sucking process, mechanical ventilation was interrupted, and the patient's airway was connected to the atmosphere. SimultaneouslySuction tubeIt also needs to be exposed to the atmosphere for operation, thus inevitably causing problems such as hypoxia and cross-infection, environmental pollution, and blood pressure and heart rhythm. In order to solve the above problems,Closed suction system(CLOSED ENDOTRACHEAL SUCTION,CES)It was successfully developed in the 1980s and began to be used clinically. It has been widely used clinically because it has the advantages of uninterrupted ventilator treatment, avoiding cross-infection and polluting the environment, and reducing the workload of nursing staff.
With Closed suction system The three links are respectively connected with the patient's artificial airway (tracheal intubation or tracheotomy), the ventilator Y-tube, and the vacuum suction device to form a closed suction system. The airway humidification joint is connected to the syringe to inject the humidification solution or drip into the humidification solution with the infusion set. Holding left while suckingSuction tubeAt the junction with the suction suction, the thumb or forefinger controls the suction valve, and the right hand is connected to the suction tube along the endotracheal tube to the required depth. Generally, the front end exceeds the front end of the tracheal intubation by ≤ 1 cm. At this time, the suction tube membrane protective sleeve is self-shrinking with the insertion of the suction tube, and the suction valve switch is pressed, and the negative pressure is sucked for 15 seconds, and the suction tube is rotated while being sucked, and the sputum is thickened to give the airway wet. Turn. After stopping the suction, the suction tube is pumped back to the black indicator line visible on the catheter, and the suction valve is pressed, and the rinsing liquid is flushed into the lumen to be rinsed for backup for next use.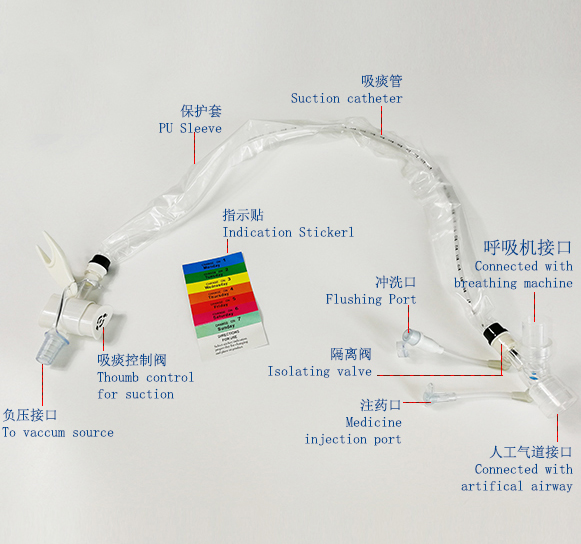
The advantages of closed suction
Compared with the open suction, the closed type reduces the operation of opening the disposable suction tube, disconnecting the ventilator, simplifying the suction process, saving time and manpower compared to the open suction, improving the work efficiency of the nurse, and Timely response to the needs of the patient for sucking. After studying 149 closed suckings and 127 open suckings in 35 patients who lived in the ICU after trauma, Johnson reported that the average duration of closed suction for each operation was 93 s, while the open suction was 153 s.
Traditional open suction is caused by a disconnection of the patient and the ventilator, resulting in a significant reduction in lung capacity, alveolar collapse, decreased arterial oxygen saturation, increased reflex heart rate, and increased blood pressure. When the closed suction is used, the patient's lung capacity is reduced less because it does not disconnect the ventilator, which is beneficial to maintain better oxygenation and prevent reflex heart rate and blood pressure. Wang Xiaoping and other 70 patients in the ICU showed that there was no significant difference in heart rhythm between patients before and after closed suction. Jongerden et al.'s study of 85 patients also showed that closed suction can significantly reduce the change of heart rhythm before and after sucking. And changes in mean arterial pressure.
Closed suction has no interruption of oxygen supply and ventilation because there is no connection to disconnect the ventilator, and there is no alveolar collapse in the preservation of lung capacity, increasing the gas exchange area and improving the oxygen saturation of the patient during sucking, so the closed type Sucking has a lower effect on blood oxygen in patients than in open sucking. Yang Xia and other research reports that closed suction in the ventilator treatment process can significantly reduce the incidence of SpO2 decline during the sucking process. According to Lee et al., closed suction has little effect on SpO2 compared with open sucking.
Closed suction prevents the patient's airway from being isolated from the outside world, preventing environmental, patient and medical personnel from being contaminated. The operation is carried out under confined conditions, avoiding the secretion of secretions to medical personnel, patients and articles, and strengthening medical care work. Security. Studies by Zhang Jin et al. show that closed suction can reduce the incidence of pollution caused by human factors and the incidence of lung infection. There are many studies on closed sputum in the prevention of nosocomial infections. Most studies have shown that the use of closed suction does not reduce the incidence of ventilator-associated pneumonia (VAP) compared with open sputum. However, it has also been reported that the use of closed suction can prevent and reduce the occurrence of VAP. Topeli et al reported that using Closed suction system caused a multi-drug resistant ventilator pipeline transplant, but did not increase the incidence of VAP.
Intracranial pressure (ICP) is an important indicator for monitoring the condition of patients with severe head injury. Intratracheal aspiration (ETS) stimulation of the trachea can cause elevated venous system pressure, which may cause patients with severe head injury to be in intracranial hypertension and cerebral ischemia. Pan Xianfang et al. showed that ICP increased after closed suction and open suction, but the cerebral perfusion pressure (CPP) increased slightly after closed suction, so it is considered that the transient ICP is elevated during closed suction. Increased mean arterial pressure can cause an increase in cerebral blood flow (CBF), thereby maintaining adequate CPP, without causing ischemia and hypoxia in the brain, while CPP is significantly decreased after open sucking, which may be due to intracranial hypertension. It is difficult for the body to quickly compensate for hypoxia during off-line attraction, and vasoconstriction and cerebral blood flow are reduced. Open-type sucking can cause cerebral ischemia and hypoxia, and the increase in ICP secondary to CBF after closed sucking does not impair cerebral perfusion, and maintains sufficient cerebral oxygen supply, compared with open sucking. It is more reasonable to apply in the state of intracranial hypertension. Therefore, for the particularity of patients with craniocerebral injury, it is recommended that clinical nurses use closed endotracheal aspiration. When the ICP is high, the suction time should be shortened, generally no more than 10 s, and the suction tube cannot be penetrated too deep to avoid stimulating the patient to cause an increase in ICP.
In the capacity control mode, due to the constant tidal volume, the inserted suction tube will increase the airway resistance, the gas exhalation will be affected, the residual gas volume will increase, and the high endogenous positive end expiratory pressure will occur, which will increase the respiratory muscle load and increase. Oxygen consumption.
Relationship between mechanical ventilation and ventilator-associated pneumonia
ICU patients often establish artificial airways for mechanical ventilation (MV) due to critical illness, but MV often causes ventilator-associated pneumonia (VAP). VAP is a common severe hospital-acquired pneumonia with an incidence of 20%. ~75%, the mortality rate is 20% to 50%, and aspiration is the main infection route of VAP. Traditional artificial airway can not remove the remnant in the subglottic space. It can only reduce the aspiration by increasing the pressure inside the balloon. However, it has many adverse reactions, which can cause compression of the tracheal mucosa, ischemia, erosion, and even tracheal esophageal fistula.
solution
The establishment of the artificial airway causes some functions of the upper respiratory tract to be lost, which affects the patient's cough ability. The conventional artificial airway is difficult to completely aspirate the secretion of the oropharynx, and the secretion enters the gap along the tracheal cannula and the tracheal wall. VAP in the respiratory tract causes death of multiple organ dysfunction. The results of this study indicate that continuous subglottic suction can pass through the lateral hole, which can absorb the secretions on the capsule, greatly reducing the occurrence of VAP and reducing mortality. The retentate above the balloon has oral nasal secretions, reflux, H2 receptor blockers in the reflux, and the acid-suppressing agent increases the pH of the stomach and increases the growth and reproduction of the G+ bacteria. Increasing the chance of infection, 62.5% of the colonization bacteria and lower respiratory tract pathogens in the retentate, is also the main cause of VAP infection. In the conventional tracheal intubation, the cystic material changes due to the position change, the airway pressure decreases, the airway diameter changes, etc. Invade the lower respiratory tract from the edge of the balloon.
Artificial airway care The most important thing in the care of artificial airways is to maintain a good filling of the artificial airbag. When the airbag of the artificial airway is inflated, it will press the wall of the trachea, thereby sealing and fixing, preventing the aspiration of the contents of the mouth and stomach. The care of such patients should adopt the minimum closure technique: after the balloon is inflated, suck When the gas is just there, no gas is exposed.
method:
Place the stethoscope on the patient's trachea and inhale the airbag while listening to the leaking sound until you can't hear the leak. Then, 0.5 ml of gas is twitched. If a small amount of air leakage can be heard, the airbag can be inflated again until no air leakage is heard during inhalation. This method can reduce the damage of the air bag to the tracheal wall to a certain extent, and is not easy to cause aspiration. The bedside of the contraindication card should be raised by 30°~45°. The airbag pressure must be strictly controlled, generally 25~35 cmH2O[2], monitored 2~3 times a day, and the pressure less than 20 cmH2O is the high risk of VAP. There may be a stagnant flow into the lower respiratory tract, the pressure is greater than 35 cmH2O, and partial compression of ischemia, necrosis, and hemorrhage should be caused to the mucosa. Pay attention to the negative pressure connection method, open the standard interface connected to the wall center negative pressure, keep the pressure between 80-150 mmHg, and continue to attract under the glottis through the elliptical opening of the catheter in the lower part of the glottis. The contraindications are between 30° and 45°.
be careful:
When the secretion is sticky or the drainage tube is blocked, the pipeline can be flushed with 5~10 ml of normal saline. Before the flushing, the airbag must be inspected to keep the airbag pressure at the upper limit of the safe pressure range. When the ventilation is flushed, the pressure above the balloon increases, so that the secretion flow enters the lower part. Respiratory tract, and adjust the balloon pressure to the patient's safe pressure range, to ensure the negative pressure under the premise of adequate drainage, VAP pathogenesis risk factors, etc., to improve prevention awareness, take comprehensive measures, oral care, anti-aspiration. Under the glottis, closed suction, pipe management, hand hygiene, environmental management, increased resistance, rest and nutrition can maximize the control of VAP.
The information comes from the public network. If there is any infringement, please contact to delete.